health
Antibiotic prescriptions for children drop by 24%
■ Prescribing rates for patients 14 and younger fell from 1993 to 2008, but antibiotic resistance is still growing.
By Christine S. Moyer — Posted Sept. 19, 2011
- WITH THIS STORY:
- » Antibiotic prescribing habits
- » External links
- » Related content
After years of doctors overprescribing antibiotics, physicians are beginning to heed experts' warnings to use the drugs more judiciously in the face of increasing antibiotic resistance, a study shows.
A Centers for Disease Control and Prevention study found that antibiotic prescribing rates for patients 14 and younger who visited a physician fell 24% from 1993-94 to 2007-08. During that period, the rate dropped from 300 antibiotic courses per 1,000 office visits to 229 courses per 1,000 visits, said the study in the Sept. 2 issue of the CDC's Morbidity and Mortality Weekly Report.
Infectious diseases experts attribute the decline largely to the efforts of health organizations, such as the American Academy of Pediatrics, to educate physicians and the public on the proper use of the drugs.
Yet more needs to be done, said lead study author Tarayn A. Fairlie, MD, MPH, an epidemic intelligence service officer in the respiratory diseases branch at the CDC's National Center for Immunization and Respiratory Diseases.
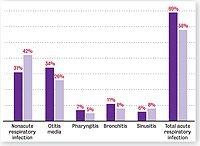
Researchers found that 58% of antibiotics prescribed in the office setting in 2007-08 were for five acute respiratory infections: bronchitis, nonspecific upper respiratory infections, otitis media, pharyngitis and sinusitis. Most episodes of these infections do not require antibiotic treatment, experts say. The prescribing figure was 69% in 1993-94.
Overall, "antibiotic prescribing has decreased, and that's great, but we really need to work on decreasing antibiotic use" for acute respiratory infections, Dr. Fairlie said. "We know inappropriate or excessive antibiotic use is a direct contribution to antibiotic resistance. Even simple infections can become much more deadly or difficult to treat."
To continue decreasing the rate of unnecessary antibiotic prescribing, health organizations should launch new initiatives that provide primary care physicians with evidence of the harms of overusing the drugs, said Harry Keyserling, MD. He is a professor of pediatrics with a specialty in infectious diseases at Emory University School of Medicine in Atlanta.
"I think one of the issues is that people get tired of the same message, so maybe we need to be creative and get better methods of communicating" this information, Dr. Keyserling said.
Resistance problems
In the United States, hospital-acquired infections kill about 90,000 people a year, according to the National Institute of Allergy and Infectious Diseases. More than 70% of the bacteria that cause these infections are resistant to at least one of the antibiotics used to treat them.
In primary care, it is not uncommon for physicians to see azithromycin-resistant streptococcus infections, Dr. Fairlie said. "We didn't see this 10 years ago."
Contributing to resistance problems are patients who do not take antibiotics as prescribed and health professionals who misuse the medication, infectious diseases experts say.
Such misuse is due in part to a lack of physician training on conserving antimicrobials, they say. Other factors include pressure from parents to prescribe antibiotics to their children and challenges in determining whether a patient's acute respiratory infection is bacterial or viral. Antibiotics are not effective against viruses.
Antibiotics also are added to livestock feed to prevent infections and increase animal growth rates. Using the drugs this way can transfer antibiotic-resistant bacteria from animals to consumers when they eat the meat products, infectious diseases experts say.
For the MMWR study, researchers analyzed data from the National Ambulatory Medical Care Survey for the period 1993-94 to 2007-08. The survey was of visits to nonfederal, office-based physicians in the U.S. The number of participating physicians for each two-year period was 2,500 to 3,500, and data were weighted to produce national estimates.
Researchers found that prescribing antibiotics for otitis media has not decreased significantly, despite the AAP's 2004 guidelines recommending watchful waiting for otherwise healthy children age 2 and older without severe symptoms or with an uncertain diagnosis.
In 1993-94, an antibiotic was prescribed for otitis media in 34% of physician visits made by children 14 and younger. The figure was 26% in 2007-08.
"I'm certainly pleased that a decrease was demonstrated" in the overall antibiotic prescribing rate, Dr. Keyserling said. "The trend is going in the right direction. But hopefully when a study is done [in the future], we will see another dramatic decrease."